Cancer and its prevalence in Australia
In Australia, according to the Australian Institute of Health and Welfare (AIHW), three out of every 10 deaths are caused by cancer, and it is estimated there were 162,163 new cancer cases diagnosed in 2022.

The treatment of cancer can become increasingly challenging as the disease progresses and spreads.
In numerous instances, cancer only presents symptoms after it has metastasised.
Therefore, early detection and screening of the asymptomatic population is crucial in preventing the disease’s advancement and achieving successful outcomes.
What is cancer screening?
Cancer screening detects early signs or risk factors for cancer, increasing treatment success and may prevent cancer.
However, further investigation is necessary for confirmation of positive findings.
There are three different approaches to screening:
- Population-based screening: This involves testing of an entire target population.
- Targeted risk screening: This involves screening high-risk individuals, such as those with a strong family history of certain types of cancer.
- Opportunistic screening: This involves screening conducted during a medical check-up, such as tests which may be ordered by a healthcare professional during an appointment for medication review or a yearly immunisation like the flu vaccine.
Three population-based cancer screening programs in Australia are free for eligible people:
- BreastScreen Australia Program: Women over 40 can have a free mammogram and women aged 50 to 74 are actively invited to screen every two years.
- National Bowel Cancer Screening Program: The Australian National Bowel Cancer Screening Program (NBCSP) provides population screening for bowel cancer free of charge to eligible people every two years for ages 50 to 74.
- National Cervical Screening Program: Women and people with a cervix aged 25 to 74 years are invited to have a Cervical Screening Test every five years through their healthcare provider.
Each program aims to detect pre-cancerous abnormalities or early-stage cancers before symptoms occur, maximising the chance of successful treatment.
Primary healthcare and its role in cancer screening
Primary healthcare providers are essential collaborators and drivers in the promotion and implementation of cancer screening programs.
Patient-centred care and participation in cancer screening programs are critical factors in decreasing cancer-related morbidity and mortality.

Studies from Cancer Institute NSW suggest the recommendation or endorsement of cancer screening programs by a primary healthcare provider elevates the participation rate in cervical, breast and bowel screening programs.
Furthermore, healthcare providers play a pivotal role in encouraging individuals to seek and engage in cancer screening programs by providing educational resources and accessible tools.
How can QIPC cancer screening module in POLAR be useful?
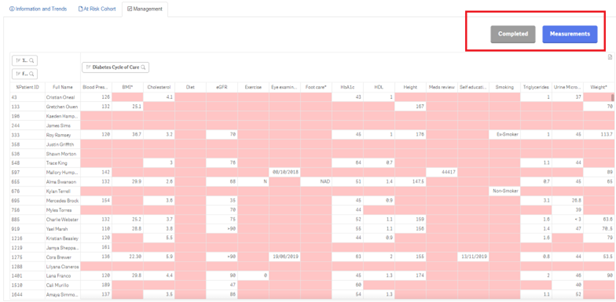
Outcome Health and SWSPHN have collaborated to develop a cancer screening module.
This module can be accessed through the POLAR QIPC report and is located under the “Clinical” tab.
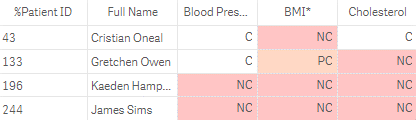
Its purpose is to help general practices identify high-risk patients who are due for screening, in order to improve their management and health outcomes.

The module has five tabs covering information and trends, cervical screening, breast screening, bowel cancer screening and skin cancer screening.
SWSPHN has created a set of POLAR Walkthroughs to assist in utilising the Cancer Screening Module effectively:
- POLAR Walkthrough – patients due for SCC or BCC review
- POLAR Walkthrough – non-urgent patients now due for bowel screen with a history of polyposis
- POLAR Walkthrough – non-urgent first nations patients due for breast screening
- POLAR Walkthrough – identifying URGENT patient cohorts in cancer screening module
Helpful tips for GPs, managers and nurses
- Private bookmark: The Private Bookmark function in POLAR allows the user to save searches of specific patient cohorts by creating a bookmark. The user can create these bookmarks at the top right-hand corner of the page. This enables the user to recall specific patient cohorts without having to re-apply filters. This can be a very effective function as it only requires the user to open the bookmarks tab and select their desired saved search.

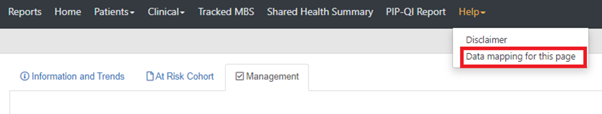
- Correct documentation: In order for POLAR to obtain precise and reliable data, it is crucial to ensure every item is accurately documented in the patient’s file. To assist clinicians and practice staff in documenting care items in the appropriate location in their clinic’s medical software, data mapping of each tab is accessible in the Help menu.

- Utilising the National Cancer Screening Register: The National Cancer Screening Register (NCSR) gives healthcare providers secure access to patient bowel and cervical screening results and histories. Providers can also submit forms and reports electronically, update patient participation details and view program-related correspondence.
- Stay current: Several resources and education opportunities are free to keep updated on the latest guidelines and information. An education space eviQ on the NSW Government site has free, evidence-based eLearning resources for health professionals.
- Providing patient education and resources: Downloadable resources for patients are available from the Cancer Council site.
- FREE cancer screening educational flipcharts: You can order free cancer screening educational flipcharts in different languages for your organisation. Click here to find more information.
- Utilising Primary Care Cancer Control Quality Improvement Toolkit: This toolkit aims to assist in incorporating cancer screening and prevention activities into your practice or health service.









 “The new principal was very focused on efficiency and data quality. The incentive payment was also just that – an incentive,” explained Walker Street General Practice manager and QI champion Emily Meadows (pictured right). Importantly, QIPC also ticked and enhanced two of Walker Street Practice’s five values. “We are committed to continuing with this as it forms a key part of two of our five values – those of Excellence and Efficiency (Teamwork, Service to Others and Honesty).”
“The new principal was very focused on efficiency and data quality. The incentive payment was also just that – an incentive,” explained Walker Street General Practice manager and QI champion Emily Meadows (pictured right). Importantly, QIPC also ticked and enhanced two of Walker Street Practice’s five values. “We are committed to continuing with this as it forms a key part of two of our five values – those of Excellence and Efficiency (Teamwork, Service to Others and Honesty).” 
 QIPC – a stepped approach for practices to improve quality of patient care
QIPC – a stepped approach for practices to improve quality of patient care